PTMC — The Life-Changing Balloon Procedure That Opens a Stiff Heart Valve (Without Surgery)
Imagine your heart’s main gate — the mitral valve — slowly rusting shut.
Every beat becomes a struggle.
Every breath, a chore.
Climbing stairs? Exhausting.
Lying down at night? Suffocating.
This is the reality for thousands living with mitral valve stenosis — often caused by untreated rheumatic fever.
But here’s the miracle of modern medicine:
You don’t need open-heart surgery to fix it.
Enter PTMC — Percutaneous Transvenous Mitral Commissurotomy — a minimally invasive, catheter-based procedure that uses a balloon to gently crack open a stiff valve… and give patients back their breath, their energy, their life.
Let’s walk through what PTMC is, why it’s revolutionary, and how it’s helping patients across Iran and beyond — one heartbeat at a time.
❤️ What Is PTMC?
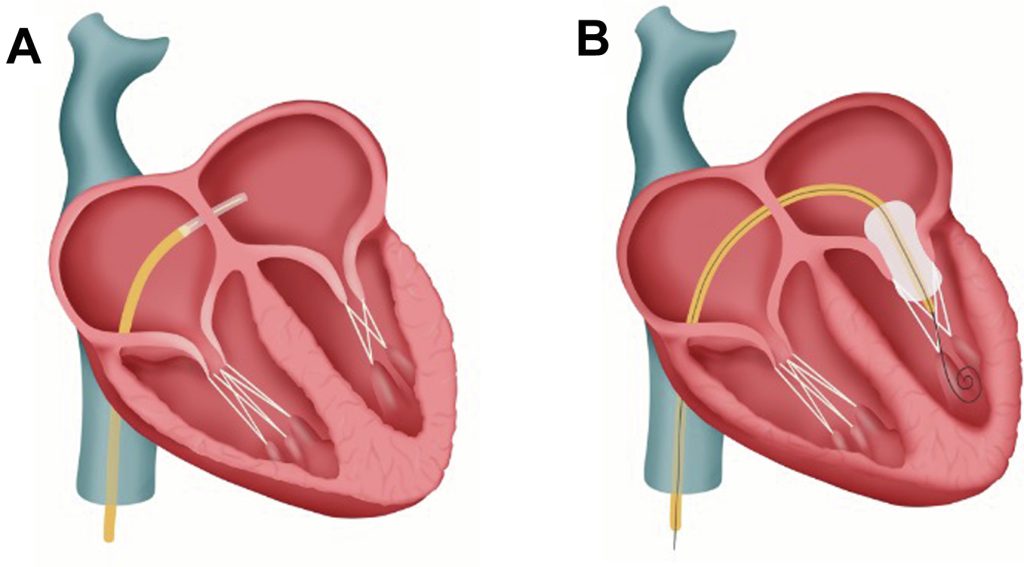
PTMC (Percutaneous Transvenous Mitral Commissurotomy) — also known as Balloon Mitral Valvuloplasty — is a non-surgical procedure to treat mitral stenosis, a condition where the mitral valve narrows and restricts blood flow from the left atrium to the left ventricle.
Instead of replacing the valve or cracking open the chest, doctors thread a special balloon-tipped catheter through a vein in your leg, guide it to your heart, and — with precision — inflate the balloon inside the valve to split open the fused leaflets.
Think of it like gently inflating a balloon inside a clenched fist — until the fingers relax and open.
⏱️ Procedure time: 30–60 minutes
🛌 Hospital stay: Usually 1–2 days
👟 Recovery: Back to light activity in days, full recovery in weeks
📊 Why Would You Need PTMC?
PTMC is recommended for patients with: 🔸 Symptomatic mitral stenosis (shortness of breath, fatigue, palpitations, swelling)
🔸 Valve area <1.5 cm² (severe narrowing)
🔸 Favorable valve anatomy (assessed by echocardiogram — leaflets not too calcified or damaged)
🔸 No left atrial clot or severe mitral regurgitation
It’s especially common in regions like Iran, India, and parts of Africa — where rheumatic heart disease remains prevalent due to past streptococcal infections.
🧪 How Does PTMC Work? Step by Step
1. Preparation
- You’ll have a detailed transesophageal echocardiogram (TEE) to check for clots and valve anatomy.
- Blood thinners may be started if needed.
- Fasting for 6–8 hours before the procedure.
2. The Procedure
- Done under light sedation or general anesthesia.
- A catheter is inserted into the femoral vein in your groin.
- Guided through the right atrium → across the atrial septum (a small puncture is made) → into the left atrium → and finally, into the mitral valve.
- A deflated balloon is positioned across the valve — then carefully inflated (sometimes in stages) to split the fused commissures.
- The balloon is deflated and removed. The septal puncture seals on its own.
3. Recovery
- You’ll rest in a monitored unit for several hours.
- An echocardiogram is done the next day to assess results.
- Most patients feel dramatic improvement within 24–48 hours.
🆚 PTMC vs. Surgical Valve Replacement
Invasiveness | Minimally invasive — no incision | Open-heart surgery |
Valve Preservation | ✅ Yes — your own valve is repaired | ❌ No — valve is replaced |
Recovery Time | Days to weeks | 6–12 weeks |
Hospital Stay | 1–2 days | 5–7+ days |
Risk | Low (rare: severe regurgitation, tamponade) | Higher (infection, bleeding, stroke) |
Durability | 5–15+ years (depends on anatomy) | 10–20+ years (mechanical/biologic) |
Best For | Younger patients, favorable anatomy | Calcified valves, severe regurgitation |
👉 Bottom line: If your valve anatomy is suitable — PTMC is the first-line treatment. It’s faster, safer, and preserves your natural valve.
🚫 Risks? Low — But Important to Understand
PTMC is very safe in experienced hands, but potential (rare) complications include:
- Severe mitral regurgitation (if valve tears too much) — may require emergency surgery
- Cardiac tamponade (fluid around the heart) — from septal puncture
- Stroke or clot — minimized by pre-procedure TEE and blood thinners
- Arrhythmias — usually temporary
💡 Good to know: Success and safety depend heavily on operator experience and proper patient selection. Always ask: “How many PTMCs has your team performed?”
🧑⚕️ What Happens After PTMC?
- You’ll start or continue medications — often including blood thinners (especially if you have atrial fibrillation).
- Follow-up echocardiograms at 1 month, 6 months, and annually.
- Most patients report: → “I can sleep flat again.”
→ “I walked up three flights without stopping!”
→ “I feel like I did 10 years ago.”
Lifestyle changes are key: avoid strep throat (to prevent recurrence), manage AFib, and stay active.
💬 Real Patient Story
“I was 32, a mother of two, and could barely carry my youngest. My doctor said my valve was ‘critically narrow.’ I was terrified of surgery. Then I had PTMC — they fixed it through my leg. I cried when I took my first deep breath afterward. Two weeks later, I danced at my cousin’s wedding. That balloon gave me my life back.”
— Narges, Rasht
✅ Final Thought
PTMC isn’t just a procedure — it’s a rescue mission for your heart.
It doesn’t replace. It repairs.
It doesn’t cut. It inflates.
It doesn’t take months. It takes minutes.
And for countless patients — especially young women, mothers, and breadwinners — it’s the difference between disability… and dignity. Between suffocation… and song.
If you’ve been diagnosed with mitral stenosis — don’t assume surgery is your only path.
Ask your cardiologist:
“Am I a candidate for PTMC?”
The answer might just open more than your valve — it might open your future.